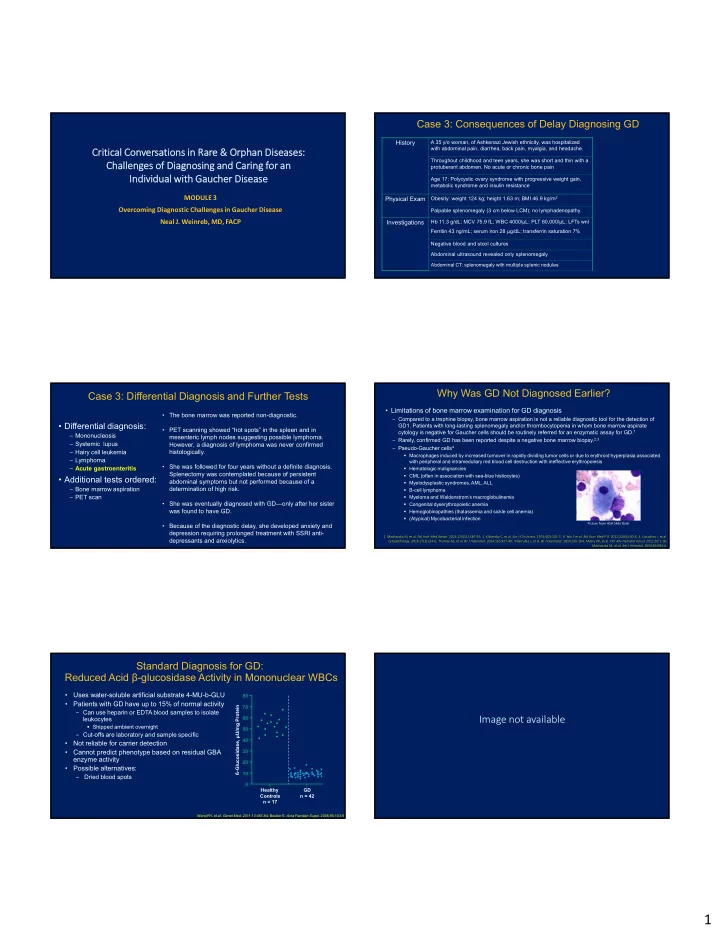
Case 3: Consequences of Delay Diagnosing GD History A 35 y/o woman, of Ashkenazi Jewish ethnicity, was hospitalized with abdominal pain, diarrhea, back pain, myalgia, and headache. Critical Conversations in Rare & Orphan Diseases: Throughout childhood and teen years, she was short and thin with a Challenges of Diagnosing and Caring for an protuberant abdomen. No acute or chronic bone pain Individual with Gaucher Disease Age 17: Polycystic ovary syndrome with progressive weight gain, metabolic syndrome and insulin resistance MODULE 3 Physical Exam Obesity: weight 124 kg; height 1.63 m; BMI 46.9 kg/m 2 Overcoming Diagnostic Challenges in Gaucher Disease Palpable splenomegaly (3 cm below LCM); no lymphadenopathy Neal J. Weinreb, MD, FACP Investigations Hb 11.3 g/dL; MCV 75.9 fL; WBC 4000/µL; PLT 60,000/µL; LFTs wnl Ferritin 43 ng/mL; serum iron 28 µg/dL; transferrin saturation 7% Negative blood and stool cultures Abdominal ultrasound revealed only splenomegaly Abdominal CT: splenomegaly with multiple splenic nodules Why Was GD Not Diagnosed Earlier? Case 3: Differential Diagnosis and Further Tests • Limitations of bone marrow examination for GD diagnosis • The bone marrow was reported non-diagnostic. – Compared to a trephine biopsy, bone marrow aspiration is not a reliable diagnostic tool for the detection of • Differential diagnosis: GD1. Patients with long-lasting splenomegaly and/or thrombocytopenia in whom bone marrow aspirate • PET scanning showed “hot spots” in the spleen and in cytology is negative for Gaucher cells should be routinely referred for an enzymatic assay for GD. 1 – Mononucleosis mesenteric lymph nodes suggesting possible lymphoma. – Rarely, confirmed GD has been reported despite a negative bone marrow biopsy. 2,3 – Systemic lupus However, a diagnosis of lymphoma was never confirmed – Pseudo-Gaucher cells 4 – Hairy cell leukemia histologically. Macrophages induced by increased turnover in rapidly dividing tumor cells or due to erythroid hyperplasia associated – Lymphoma with peripheral and intramedullary red blood cell destruction with ineffective erythropoiesis • She was followed for four years without a definite diagnosis. – Acute gastroenteritis Hematologic malignancies Splenectomy was contemplated because of persistent CML (often in association with sea-blue histiocytes) • Additional tests ordered: abdominal symptoms but not performed because of a Myelodysplastic syndromes, AML, ALL – Bone marrow aspiration determination of high risk. B-cell lymphoma – PET scan Myeloma and Waldenstrom’s macroglobulinemia • She was eventually diagnosed with GD—only after her sister Congenital dyserythropoietic anemia was found to have GD. Hemoglobinopathies (thalassemia and sickle cell anemia) (Atypical) Mycobacterial infection Picture from ASH Slide Bank • Because of the diagnostic delay, she developed anxiety and depression requiring prolonged treatment with SSRI anti- 1. Machaczka M, et al. Pol Arch Med Wewn . 2014;124(11):587‐92; 2. Klibansky C, et al. Eur J Clin Invest . 1974;4(2):101‐7; 3. Ysla F et al. Bol Asoc Med P R . 2012;104(4):50‐3; 4. Cozzolino I, et al. depressants and anxiolytics. Cytopathology. 2016;27(2)134‐6; Thomas AS, et al. Br J Haematol . 2014;165:427‐40; Villarrubia J, et al. Br J Haematol . 2014;165:164; Mistry PK, et al. Clin Adv Hematol Onco l. 2012;10:1‐16; Machaczka M, et al. Am J Hematol . 2009;84:694‐6. Standard Diagnosis for GD: Reduced Acid β-glucosidase Activity in Mononuclear WBCs • Uses water-soluble artificial substrate 4-MU-b-GLU 80 • Patients with GD have up to 15% of normal activity 70 ß-Glucosidase, µU/mg Protein – Can use heparin or EDTA blood samples to isolate 60 Image not available leukocytes Shipped ambient overnight 50 – Cut-offs are laboratory and sample specific 40 • Not reliable for carrier detection • Cannot predict phenotype based on residual GBA 30 enzyme activity 20 • Possible alternatives: 10 Dried blood spots – 0 Healthy GD Controls n = 42 n = 17 Wang RY, et al. Genet Med . 2011;13:457-84; Beutler E. Acta Paediatr Suppl . 2006;95:103-9. 1
Why Was GD Not Diagnosed Earlier? Why Was GD Not Diagnosed Earlier? Differential diagnosis—other more common hematologic diseases It’s not on the diagnostic radar! GD 1 CML ALL NHL MM ITP Typical age 0-80+ 2-3 2-3 55-60 70 30-40 Only 1 out of 5 hematologists suspected GD in a patient with 6 of the most common signs and symptoms of GD at diagnosis (children) (children) >65 63 (adults) (adults) Bone pain ‒‒ Conditions that physicians suspected when presented with a case of a Bruising/bleeding 42-year-old man presenting with anemia, thrombocytopenia, hepatomegaly, splenomegaly, Proportion of Physicians acute bone pain, and chronic bone pain Fatigue Hepatomegaly Less Rare common Splenomegaly Less Rare common Gaucher cells on In clusters Pseudo- Pseudo- Pseudo- Pseudo- No biopsy Gaucher Gaucher Gaucher Gaucher cells cells cells cells Leukemia Lymphoma MM GD CGL Other Bleeding No Answer Disorders MM, multiple myeloma; GD, Gaucher disease; CGL, chronic granulocytic leukemia Thomas AS, et al. Blood Cells Mol Dis . 2013;50:212-7; Mistry PK, et al. Am J Hematol . 2007;82:697-701. Mistry PK, et al. Am J Hematol. 2007;82;697-701. Story of a Diagnostic and Therapeutic Odyssey: Implications of Missed Diagnosis An Ashkenazi Jewish Woman (N370S/N370S) • “ When I was 10 y/o, I began to experience terrible pains in my • When a GD diagnosis is missed: legs. My mother thought that these were growing pains and left it – A patient may experience delays for up to 10 years until a correct diagnosis at that. But, as I grew older, my pain symptoms worsened and, in is rendered. addition, I had severe bleeding episodes as well as bouts of – GD is progressive over time and, if left untreated, may lead to: fatigue. I used to think I was the laziest person in the world • Premature death from bleeding complications because I felt so lethargic and tired. • Pulmonary hypertension • Liver disease Through the following years, the cause of the symptoms was never properly diagnosed. It was only at age 23, right after my marriage, that a hematologist finally gave my disease a • Sepsis name, Gaucher disease, and recommended removal of my spleen. My husband and I were • Growth failure against this and so I remained with my symptoms unabated. I still vividly remember how I had • Complications from advanced bone disease hemorrhage for 17 days in the hospital after the birth of my first child.” • Negative effect on quality of life Thomas AS, et al. Blood Cells Mol Dis . 2013;50:212-7; Mistry PK, et al. Am J Hematol . 2011;86:110-5; Mistry PK, et al. Am J Hematol . 2007;82:697-701. Story of a Diagnostic and Therapeutic Odyssey: Points to Remember An Ashkenazi Jewish Woman (N370S/N370S) “Relief finally came after we retired and moved to Florida in 1980 where I was referred by my cardiologist to [a Gaucher disease expert]. He helped me manage my disease and gave me • Gaucher disease shares many features in common with other benign and medicine to treat my pains, but we were both frustrated because there was still no other real malignant illnesses. treatment. In 1991, I started treatment with alglucerase*, the enzyme that had just become available for • Before GD is ever considered, hematologic malignancy is often suspected and treating Gaucher disease. It took a while for me to respond because my platelets were very low, the diagnosis of GD is then discovered serendipitously. but after about 3 years, even the platelet count was a lot better. • Most physicians, including hematologists, do not think of GD sufficiently early in I was eventually switched to imiglucerase, the newer version of the enzyme, and have been on the diagnostic process to avoid testing that may be unnecessary. treatment now for more than 13 years. (2005). It has helped me tremendously, alleviating bone pain and fatigue symptoms. I still occasionally have bleeding problems but that is mainly due to • Diagnostic odysseys, delayed diagnosis and procrastination in starting treatment medication that I have to take for my heart. can lead to chronic patient anxiety as well as irreversible complications, Through the years, I have had several major surgeries, and had I not been treated for the Gaucher significant morbidity and even premature mortality. disease, I would have had severe complications or worse. I feel fortunate to lead a normal life at 81 years of age. I read, keep busy and have a positive attitude.” Patient died in 2011 at age 88 of renal failure and CHF. *Withdrawn from market. 2
Points to Remember (continued) • Testing for GD should be considered in any person presenting with combinations of bone pain, hepatosplenomegaly, or hematologic cytopenias. • Bone marrow aspiration and biopsy can yield false diagnostic positives and false diagnostic negatives. • The gold standard for diagnosis is measuring leukocyte acid β-glucosidase activity, which is typically <10% of control values. • Bone marrow examinations are not a necessary part of a work up for GD unless a concurrent hematologic disorder such as myeloma is suspected based on clinical or laboratory evidence. 3
Recommend
More recommend